

The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.Ĭompeting interests: The authors have declared that no competing interests exist.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.ĭata Availability: All available data are presented as supplementary tables.įunding: SL: Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (grant number: 2017R1E1A1A01074324). Received: SeptemAccepted: DecemPublished: January 24, 2019Ĭopyright: © 2019 Lee et al. PLoS ONE 14(1):Įditor: Niels Bergsland, University at Buffalo, UNITED STATES (2019) Which brain lesions produce spasticity? An observational study on 45 stroke patients. These results may be useful for planning rehabilitation strategies and for understanding the pathophysiology of spasticity in stroke patients.Ĭitation: Lee KB, Hong BY, Kim JS, Sul B, Yoon SC, Ji E-K, et al. Specifically, the involvement of white matter tracts and the striatum influenced the development of spasticity in the upper and lower limbs of stroke patients. The present study identified several brain lesions that contributed to post-stroke spasticity. Additionally, lesions of the superior corona radiata, posterior limb of the internal capsule, caudate nucleus, posterior corona radiata, thalamus, putamen, and external capsule were associated with the development of lower-limb spasticity. The VLSM method with non-parametric mapping revealed that lesions in the superior corona radiata, posterior limb of the internal capsule, posterior corona radiata, thalamus, putamen, premotor cortex, and insula were associated with the development of upper-limb spasticity. Spasticity developed to a certain degree within 3 months in most stroke patients with spasticity.
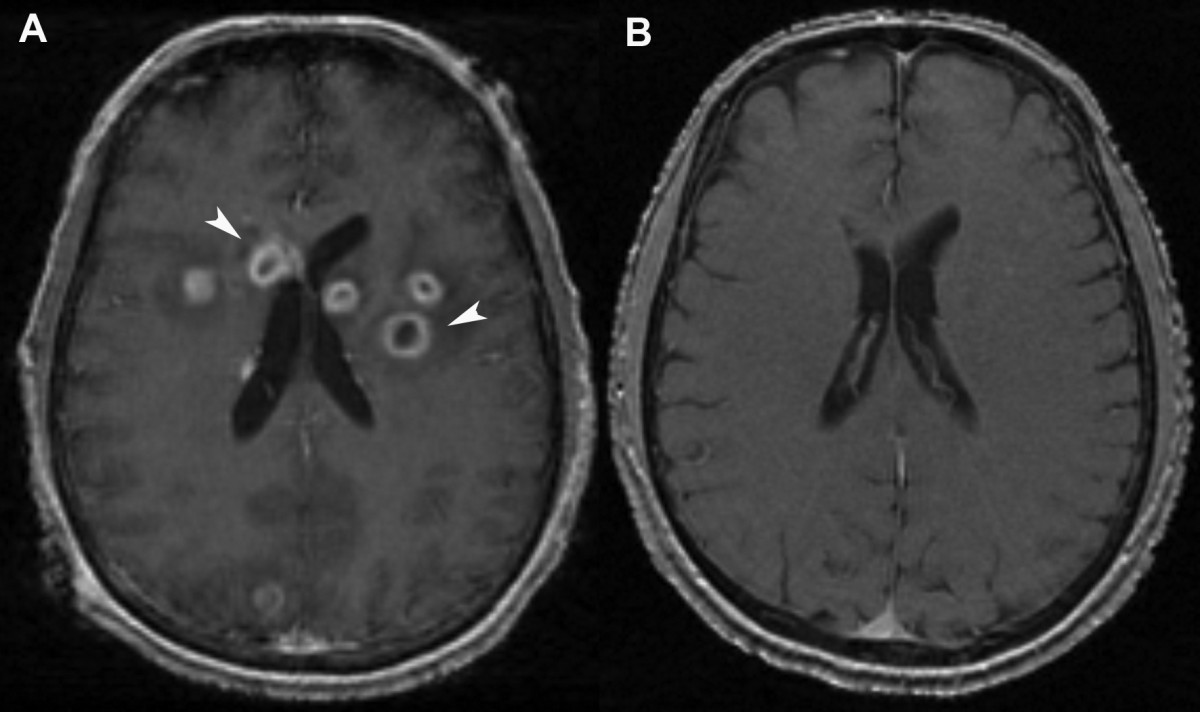
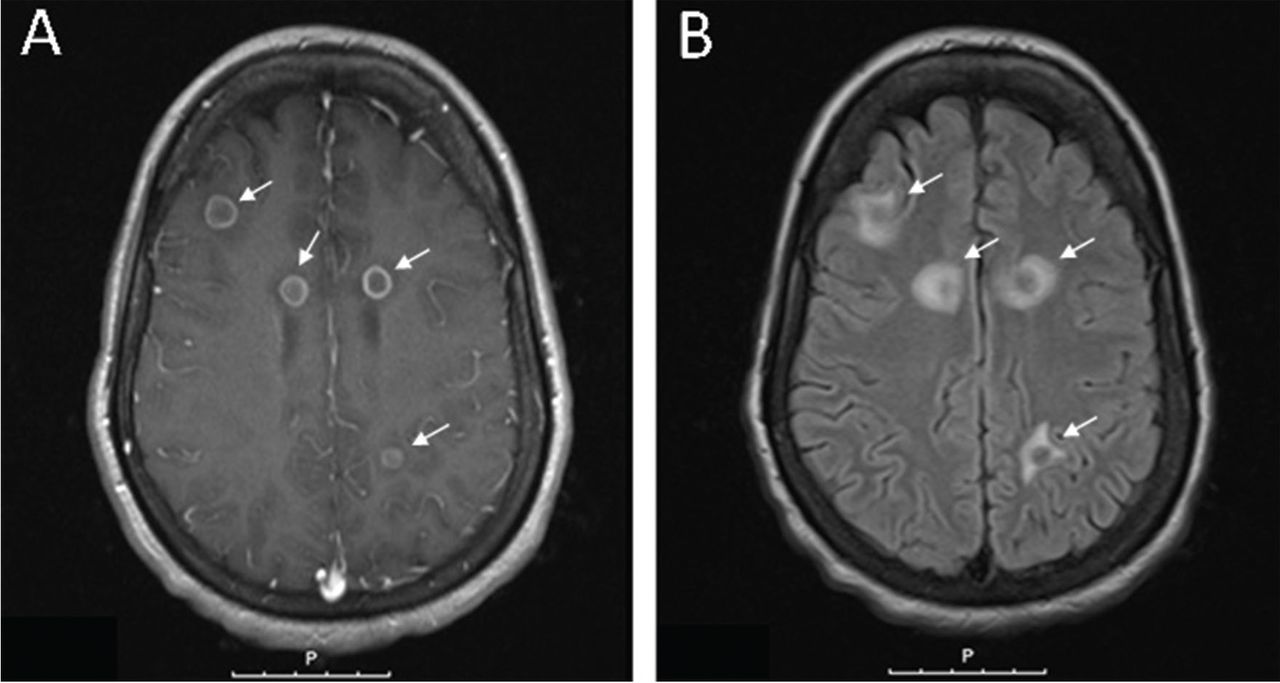
Brain lesions were analyzed using voxel-based lesion symptom mapping (VLSM) with magnetic resonance imaging images. Each patient was assessed four times: initially (within 2 weeks of stroke) and at 1, 3, and 6 months after the onset of stroke. The present retrospective longitudinal observational study assessed 45 stroke patients using the modified Ashworth Scale to measure muscle spasticity. Thus, the present study investigated the effects of stroke lesions on spasticity in stroke patients. Although several studies have attempted to elucidate the relationship between brain lesions and spasticity, the effects of specific brain lesions on the development of spasticity remain unclear. Spasticity is an important barrier that can hinder the restoration of function in stroke patients.


 0 kommentar(er)
0 kommentar(er)
